Celebrating mental health heroes
During the COVID-19 pandemic, the people implementing the Mayor’s Office of Community Mental Health programs — including clinicians, social workers, data analysts, and many others — are going above and beyond to provide mental health services for New Yorkers in need.
For some, this means offering grief counseling to students and families. For others, it means implementing new safety protocols when responding to mental health crises in people’s homes. We are grateful to these heroes for showing commitment and courage during a time of great uncertainty and profound mental health needs in our city.
Social work in the park
Florie St. Aime, Clinical Social Work Manager

When COVID-19 first hit Brooklyn’s Red Hook community in March, Florie St. Aime found new ways to reach her neighbors with help and support.
Every Wednesday Florie, a Clinical Social Work Manager at the Red Hook Initiative (RHI), brought a table to Coffey Park. There, she and her counseling team sat and talked with community members about the challenges they were experiencing during the pandemic. Equipped with flyers and stress balls, and willing to chat with anyone who was struggling with anxiety or loss, Florie was there to provide immediate support and connection to ongoing services. The weekly event – called “Social Workers in the Park” – immediately proved to be a safe and effective way of being there for the Red Hook community. The initiative continues now every week at RHI Farms.
“Florie always takes initiative,” said Ericka Medina, Senior Director of Programs at the Red Hook Initiative. “She pushes her vision forward to make it a reality. She’s inspiring.”
This is not the first time RHI has helped its neighbors pull together in a crisis. The organization has built strong ties with the Red Hook community through youth development programs, community organizing initiatives, and local hiring. When Hurricane Sandy devastated Red Hook in 2012, RHI’s deep community roots helped it become a hub for relief and rebuilding work. Today, RHI is once again helping Red Hook weather a disaster, coordinating a local response to the COVID-19 pandemic.
A native Brooklynite, Florie plays an important role in this work, helping Red Hook residents get the mental health support they need through an organization they trust. That’s what the Connections to Care program is all about – embedding mental health capacity in community-based organizations to reach more people, right in their neighborhoods.
Florie trains her colleagues to integrate mental health approaches into their day-to-day interactions with clients, which have become increasingly important this year. And to ensure that Red Hook residents have access to trauma-informed mental health support in this difficult time, Florie continues to embrace new approaches – whether it’s providing tele-mental health services, launching an acupuncture healing initiative, or tabling at the park. She remains committed to doing everything she can to support the well-being of her neighbors.
“Florie looks at the individual as a family member or community member,” said Ericka Medina, Senior Director of Programs at Red Hook Initiative. “She asks—how does this person heal?”
From Florie:
“I root my work in naming and blaming social constructs instead of individuals; encouraging healing and self-care as resistance; and reintroducing human connection and acts of love as radical action.”
The Mayor’s Office of Community Mental Health program: Connections to Care: Mental Health Integration in Community-Based Organizations
The Mayor’s Office of Community Mental Health partners with the Mayor’s Office for Economic Opportunity to integrate mental health support into the work of community-based organizations (CBOs) serving at-risk and low-income communities across the City. Through Connections to Care, CBO partners work with mental health providers who train and coach staff to screen their clients for mental health needs, offer direct support when appropriate, and link to local health providers for further care if needed. The program is operated in partnership with the Department of Health and Mental Hygiene, with additional funding through the Mayor’s Fund to Advance New York City and other private funders. Nearly 2,000 community-based staff have been trained through the program, and more than 46,000 New Yorkers have received screening or other services. More than 80 percent of clients referred to mental health services at the height of the pandemic (April through June 2020) kept their appointment. Learn more about the program and its impact here.
Support in their darkest moments and happiest successes
Morgan Siegel, Health and Wellness Program Manager

As a bilingual therapist at the community nonprofit NMIC, Morgan Siegel has seen firsthand that communities of color, including the Latinx communities in upper Manhattan and the Bronx, are bearing a particularly heavy mental health burden during the COVID-19 pandemic. She has spent the last several months directly addressing this profound need.
Ms. Siegel manages NMIC’s Connections to Care program, a Mayor’s Office of Community Mental Health initiative that helps non-profit organizations embed mental health support into the services they offer their communities. Under Ms. Siegel’s leadership, the program provides bilingual counseling and referrals, and also trains NMIC staff to screen clients for mental health needs and connect them to clinical services.
As COVID-19 cases spiked through the City, Ms. Siegel moved her team’s services from in-person to virtual in order to keep her clients safe. This was no small feat: some clients needed extra support adapting to tele-mental health technology, and many had trouble finding time and space to speak privately in multi-family households. Despite the challenges, the transition to tele-mental health has been remarkably successful: 93% of clients referred to mental health services by NMIC have kept their appointments during the pandemic.
Ms. Siegel knew that it wasn’t just clients who needed mental health support, her colleagues did as well. She developed virtual groups for NMIC staff who were feeling COVID-related stress and anxiety, so they could connect while remaining physically apart. “It’s been wildly popular with staff,” said Rodrigo Sanchez-Camus, Director of Legal, Organizing, & Advocacy Services. “Staff felt a lot of pressure and needed an outlet.”
Her work didn’t end there. During the summer, when the death of George Floyd sparked protests around the City, Ms. Siegel wanted other NMIC staff members to consider the ways in which issues of systemic inequity and racist violence could be viewed through the lens of mental health. She launched a series of internal staff conversations to help NMIC explore how to best serve their clients through a race-informed therapeutic approach.
“Morgan’s internal focus on mental health work has been transformational in that she’s led robust conversations about how we approach our clients and communicate with them,” added Rodrigo Sanchez-Camus. “We wouldn’t have been able to do that without Connections to Care and without Morgan. Our agency is blessed to have her.”
From Ms. Siegel:
“I knew my entire life that I would be in a helping profession. I love to walk alongside clients in their journey through their darkest moments and happiest successes. During this time, when mental health is now more important than ever, I have felt the power of a program to provide supportive and responsive services to our community.”
The Mayor’s Office of Community Mental Health program: Connections to Care: Mental Health Integration in Community-Based Organizations
The Mayor’s Office of Community Mental Health partners with the Mayor’s Office for Economic Opportunity to integrate mental health support into the work of community-based organizations (CBOs) serving at-risk and low-income communities across the City. Through Connections to Care, CBO partners work with mental health providers who train and coach staff to screen their clients for mental health needs, offer direct support when appropriate, and link to local health providers for further care if needed. The program is operated in partnership with the Department of Health and Mental Hygiene, with additional funding through the Mayor’s Fund to Advance New York City and other private funders. Nearly 2,000 community-based staff have been trained through the program, and more than 46,000 New Yorkers have received screening or other services. More than 80 percent of clients referred to mental health services at the height of the pandemic (April through June 2020) kept their appointment. Learn more about the program and its impact here.
Housing, meals, cell phones, medication – whatever clients needed
Bridgette Callaghan, Program Director for Intensive Mobile Treatment

Throughout the pandemic, as many service providers switched to tele-mental health services, Bridgette Callaghan and her team continued to hit the streets to deliver in-person mental health treatment to vulnerable New Yorkers.
Ms. Callaghan leads the Institute for Community Living’s (ICL) Brooklyn Intensive Mobile Treatment (IMT) team, made up of mental health and substance use professionals who provide ongoing, clinical treatment to people in their communities. Clients typically have had recent contact with the criminal justice system, have serious mental health needs, and may be experiencing homelessness or substance use. ICL’s team meets with clients regularly to bring them medication and other support as well as connect them to essential services, like housing and meals.
During the pandemic, Ms. Callaghan and her team went above and beyond to make sure that clients had the care they needed. They purchased phones for clients who couldn’t afford them, so they could continue to receive services remotely. For others who preferred in-person care, they continued traveling to these clients to deliver treatment—even when that meant going as far as two hours away upstate.
Ms. Callaghan’s daily outreach helps her build strong relationships with her clients. Some even view her as family. Over the summer, one client, a young woman in her twenties, urgently needed housing. She turned to Ms. Callaghan, who helped her adhere to the treatment plan necessary to qualify for supportive housing. Ms. Callaghan takes real satisfaction in helping her clients, and her team follows her lead.
“Bridgette gets a lot of gratification from working with people others may have trouble working with,” said Jose Cotto, Vice President, Treatment & Recovery Services at ICL, Inc. “She can empathize with people on a level that other people can’t. Whereas other people would quickly give up when someone says ‘I don’t want to work with you,’ Bridgette hears, ‘I’m in pain, or I’m isolated.’ That’s why she’s able to provide really great work.”
Another testament to Ms. Callaghan’s leadership: since ICL’s Brooklyn IMT team was created two years ago, nearly everyone she has hired still works on her team. This is impressive because the work can be emotionally challenging, especially during a pandemic. As team leader, Ms. Callaghan ensures that her colleagues are able to process their emotions before going back into the field. This exemplifies Ms. Callaghan’s approach: a deep commitment to the well-being of her team and her clients underlies everything she does.
From Ms. Callaghan:
“Every day I wake up proud to call myself a social worker. I am honored to have the opportunity to work in this field and have a positive impact on the lives and communities of others.”
The Mayor’s Office of Community Mental Health program: Intensive Mobile Treatment
The Mayor’s Office of Community Mental Health partners with the Department of Health and Mental Hygiene to support Intensive Mobile Treatment (IMT) teams of mental health, substance use and peer specialists. IMT teams provide intensive and continuous support and treatment to individuals with serious needs, where and when they need it. Clients have been poorly served by traditional treatment models, have had recent behavior that is unsafe and escalating, and have had frequent contact with the mental health, criminal justice, and homeless services systems. IMT teams have maintained very high levels of client retention during the COVID-19 pandemic, serving as many people at any given time during the pandemic as before. Ninety percent of people served by IMT have continued to receive services for a year or more, and more than 50 percent of clients experiencing homelessness have secured permanent non-shelter housing while receiving treatment from an IMT team. Learn more about the program and its impact here.
Assembling an all-star team to help New Yorkers in need
Roshni Misra, Program Director for Intensive Mobile Treatment

As the Program Director of Intensive Mobile Treatment (IMT) at the Center for Urban Community Services (CUCS), Roshni Misra is used to a busy workload. Just as the COVID-19 pandemic began in New York City, she received the opportunity to create a second mobile treatment team. Ms. Misra went into overdrive to make sure both teams were in the field serving New Yorkers at a time of unprecedented need.
This meant navigating the entire hiring process remotely. IMT teams, like the two Ms. Misra leads in Manhattan, provide intensive, individualized care to clients who have had contact with the criminal justice system, may be experiencing homelessness, and have serious mental health needs. It takes specialized experience and ability to serve on the teams, so the hiring process is especially important.
Ms. Misra conducted interviews on Zoom, trained her new team members on top of her existing responsibilities in the field, and also introduced nine new team members to one another, none of whom had ever worked together before. Almost immediately, they were called into action.
When the subways closed for extensive cleaning in the spring, the team engaged a client who had experienced homelessness for 12 years and sometimes slept on the subways. The client had a very serious medical problem, and the team was determined to help him get the care he needed. One team member took him to a clinic and spent six hours with the client to make sure he received testing to better understand his medical needs.
The client went missing in the subsequent days, but the team located him once again. And with the help of Bellevue Hospital, the Safe Haven, and a homeless outreach team, he finally received the medical treatment he needed. Ms. Misra felt proud of the team she had only just assembled, noting that she had never seen people work so collaboratively and well together. Her supervisors weren’t surprised – they believe the team’s success is a testament to the strength of Ms. Misra’s leadership.
“Roshni has a firm value structure and commitment to helping people who maybe have been left out of things in life,” said Julie Lorenzo, Chief Program Officer at CUCS. “She’s committed to social justice and equality and that informs everything she does every day.”
“She’s the best person to run a program like this in a time like this,” added Mary Taylor, Chief Development and Communications Officer at CUCS. “She looks at every person, whether a staff person or a person being treated in the IMT program, with dignity and respect.”
From Ms. Misra:
“I am always proud of the services our team provides, but I have been re-inspired watching my teams’ fierce dedication to ensuring our participants still feel connected. Despite the challenges, the teams have been committed to doing essential visits and figuring out ways to provide care in new and creative ways. Whether it is engaging a new participant on the street for the first time or making sure a participant who was previously receiving weekly visits still feel they have support, IMT is there. Reading a participant a book over FaceTime, delivering groceries and medications, and bringing blankets to the hospital for someone after surgery are just a few ways the team did this.”
The Mayor’s Office of Community Mental Health program: Intensive Mobile Treatment
The Mayor’s Office of Community Mental Health partners with the Department of Health and Mental Hygiene to support Intensive Mobile Treatment (IMT) teams of mental health, substance use and peer specialists. IMT teams provide intensive and continuous support and treatment to individuals with serious needs, where and when they need it. Clients have been poorly served by traditional treatment models, have had recent behavior that is unsafe and escalating, and have had frequent contact with the mental health, criminal justice, and homeless services systems. IMT teams have maintained very high levels of client retention during the COVID-19 pandemic, serving as many people at any given time during the pandemic as before. Ninety percent of people served by IMT have continued to receive services for a year or more, and more than 50 percent of clients experiencing homelessness have secured permanent non-shelter housing while receiving treatment from an IMT team. Learn more about the program and its impact here.
Delivering a much-needed human touch
Jairu Siwazuri, Mental Health Nurse and Derrick Brown, Peer Support Specialist
The Center for Alternative Sentencing and Employment Services (CASES) provides supportive services for people with criminal justice involvement and behavioral health needs to help maximize their opportunities for success. One critical form of support CASES offers is an Intensive Mobile Treatment (IMT) team that provides intensive, highly-catered care to clients with serious mental illness. Jairu Siwazuri and Derrick Brown, two IMT team members at CASES, worked hard to reach and serve clients despite the obstacles created by the COVID-19 pandemic.
With nine team members, IMT teams include a nurse like Mr. Siwazuri and peer specialists like Mr. Brown. Each member of the team works with clients in different capacities. As the team’s nurse, Mr. Siwazuri was committed to serving clients in person, even when that meant traveling to COVID-19 hotspots. Donned in full PPE, he met clients five days of the week to deliver medications and connect them to vital services like meals and shelter, especially as the pandemic intensified.
One of those clients was an older man who had an array of mental health and physical health issues. When Mr. Siwazuri began to work with him, he had Hepatitis C, struggled with substance use, and needed an operation for a medical problem in his eye. Since then, Mr. Siwazuri has accompanied him to every appointment, administered his medication, and made the necessary arrangements for his eye operation. In recent months, the man celebrated a year of sobriety, thanks, in part, to Mr. Siwazuri’s steadfast support.
“We believe this client would not be alive if it weren’t for Jairu,” said Patricia Haversham- Brown, Director of Intensive Mobile Treatment at CASES. “I always say, I wish he was my nurse – and that says everything you need to know about him.”
As the team’s peer specialist, Derrick Brown has been an equally important source of support for IMT clients.Although Mr. Brown first started on the team as an intern, he quickly built bonds with clients by drawing on his experience with homelessness, the criminal justice system, and his path toward recovery. He’s often the first person a client meets when referred to IMT, and he’s developed a knack for breaking barriers with reluctant clients. As the COVID-19 pandemic hit its peak in the spring and some clients refused to wear masks, Mr. Brown was able to explain why it was so important to their health and safety—eventually convincing them to cooperate.
“Derrick is able to share himself in a beneficial way to reduce the substance use, mental health, homeless, and criminal justice stigmas that are part of his clients’ history,” Haversham-Brown said. “He can show them, ‘This is where I am, and this is where I’ve come from,’ to give them an opening to see they can also change their lives.”
When the pandemic hit, both Mr. Siwazuri and Mr. Brown delivered in-person support to clients—a much-needed human touch—at a time when many health services were transitioning to remote care. Director Haversham-Brown says that this in-person support makes all the difference in the lives of vulnerable New Yorkers with serious mental illness: “If we think about how it is for us, in a house by ourselves, think about how it is for them in a shelter, in a room by themselves. To be able to see someone and what they may need, the lightbulb goes off.”
From Mr. Siwazuri:
“I became a Mental Health Nurse to address disparities faced by my clients. It has been a pleasure to provide care to my clients that focuses on their mental health, medical, and social needs. The best part of my job is witnessing progress throughout their healthcare journeys.”
From Mr. Brown:
“I do this work because I’ve been through some of the same situations as the clients I serve. Anything is possible!”
The Mayor’s Office of Community Mental Health program: Intensive Mobile Treatment
The Mayor’s Office of Community Mental Health partners with the Department of Health and Mental Hygiene to support Intensive Mobile Treatment (IMT) teams of mental health, substance use and peer specialists. IMT teams provide intensive and continuous support and treatment to individuals with serious needs, where and when they need it. Clients have been poorly served by traditional treatment models, have had recent behavior that is unsafe and escalating, and have had frequent contact with the mental health, criminal justice, and homeless services systems. IMT teams have maintained very high levels of client retention during the COVID-19 pandemic, serving as many people at any given time during the pandemic as before. Ninety percent of people served by IMT have continued to receive services for a year or more, and more than 50 percent of clients experiencing homelessness have secured permanent non-shelter housing while receiving treatment from an IMT team. Learn more about the program and its impact here.
She radiates energy and positivity
Sandy Lulu, Licensed Clinical Social Worker

Sandy Lulu, an Arab-American woman, grew up speaking Arabic, which enabled her to have a strong connection to her community and culture. Today, Ms. Lulu is a licensed clinical social worker at Family Health Centers of NYU Langone, where she provides services to the most vulnerable communities.
When Ms. Lulu first learned of the opportunity to partner with the Arab American Association of New York (AAANY) to support building their mental healthcare services through Connections to Care (C2C), she knew she had to be part of the project. Over the past five years, Ms. Lulu helped design and expand the Mental Health Program at AAANY, proving to be a perfect fit. She has given 110% of her effort and worked tirelessly for her community by providing essential services during the COVID-19 pandemic – a most challenging period.
Before the COVID-19 pandemic began, Ms. Lulu’s first task with AAANY consisted of getting their staff up to speed on mental health basics so they could integrate a mental health approach in their day-to-day interactions with clients. Ms. Lulu trained all staff members and volunteers on psychoeducation, motivational interviewing, Mental Health First Aid, and screening and assessing clients for mental health needs. She ensured that cultural and linguistic sensitivity were at the forefront of every training.
When the COVID-19 pandemic struck, AAANY staff were prepared to respond to mental health needs in the community, thanks to the efforts of Ms. Lulu and other team members. In addition to training and coaching staff, Ms. Lulu began providing support to the social workers-in-training and the case managers at AAANY. Ms. Lulu designed and co-led workshops for participants on mental health awareness, domestic violence, and substance use issues during COVID-19, and shared educational information with her clients so they could protect themselves from the virus. Looking ahead to the long-term mental health effects of the pandemic, Ms. Lulu also spearheaded an effort to educate people on the importance of remaining engaged in mental health services as a community to protect their physical and mental health.
Furthermore, Ms. Lulu made sure that systems and tools were in place to address her clients’ immediate and long-term mental health needs. She established referral partnerships with other community providers at NYU Langone, specifically with other mental health professionals who spoke Arabic and understood the Arabic Community. Additionally, she volunteered in food distribution, providing essential basic nutrition packages to those experiencing food insecurities. Ms. Lulu’s pioneering work at AAANY has provided the structure and blueprint in place to meet their clients’ mental health needs during this pandemic and its unseen effects.
“I don’t know anyone who will go to the extent that Sandy will go for the community,” said Dr. Joseph Laino, Assistant Director of Clinical Services at Family Health Centers of NYU Langone Sunset Terrace. “She identifies as part of the community herself, and she’s so committed they get the services they need. She’ll get up at 5 in the morning to polish a PowerPoint presentation. She just radiates energy and positivity.”
From Ms. Lulu:
“As a Palestinian-American woman and a clinical social worker, I find myself in a position of privilege to serve my community. The guiding principles of compassion, preventing hardship, and empowering others are core cultural and spiritual values that have been instilled in me since childhood. I wouldn’t be able to do the work that I do without the support of the fantastic team of AAANY, my colleagues, friends and family. I am humbled by this honor.”
The Mayor’s Office of Community Mental Health program: Connections to Care: Mental Health Integration in Community-Based Organizations
The Mayor’s Office of Community Mental Health partners with the Mayor’s Office for Economic Opportunity to integrate mental health support into the work of community-based organizations (CBOs) serving at-risk and low-income communities across the City. Through Connections to Care, CBO partners work with mental health providers who train and coach staff to screen their clients for mental health needs, offer direct support when appropriate, and link to local health providers for further care if needed. The program is operated in partnership with the Department of Health and Mental Hygiene, with additional funding through the Mayor’s Fund to Advance New York City and other private funders. Nearly 2,000 community-based staff have been trained through the program, and more than 46,000 New Yorkers have received screening or other services. More than 80 percent of clients referred to mental health services at the height of the pandemic (April through June 2020) kept their appointment. Learn more about the program and its impact here.
Style and grace in a moment of chaos
Marge Keiser, Early Childhood Social Worker, Brooklyn

Marge Keiser, an Early Childhood Social Worker at the Department of Education, goes out of her way to make a personal connection with everyone she meets in the course of her work. When the pandemic hit, it was no surprise that Ms. Keiser made it her priority to stay connected with the children and families she serves.
Before becoming a social worker, Ms. Keiser worked as a Parent Coordinator in the same Northern Brooklyn neighborhood she now serves. It’s also the same neighborhood where she raised her three children. She knows the community well, and she has deep compassion for the families who have struggled with school closures during the pandemic. Ms. Keiser’s commitment led her to meet families where they were during this difficult time by offering support at flexible hours and providing multiple ways for families to get in touch with her.
“She wanted caregivers to know that she was there for the schools, but she was also there for them,” said Laura Colevecchi, Mental Health and Wellness Administrator, Division of Early Childhood, Brooklyn North. “Marge understands the needs of young children and she understands the challenges parents and caregivers may have as well.”
Ms. Keiser takes a whole-family approach to her work, helping both caregivers and children understand how children handle stress, and helping parents and caregivers accept that it was okay for them to be anxious, too.
“She has a sage-like quality about her, a way of making folks feel comfortable,” said Ms. Colevecchio. “She had style and grace during a moment of chaos and unknowns.”
From Ms. Keiser:
“I am drawn to this work by the possibilities of empowering people and programs to grow personally and professionally, and the opportunity to do it every day.”
The Mayor’s Office of Community Mental Health program: Social Emotional Learning
Social, emotional, and behavioral regulation skills are foundational for learning and well-being. Through a partnership between The Mayor’s Office of Community Mental Health and the Department of Education, Pre-K and 3-K programs across New York City provide social-emotional learning support to students, families, program leaders and teaching teams. Over 3,000 schoolteachers or program staff participated in at least one professional learning through this program since the program launched in 2016. And, an additional 3,000 parents and caregivers have attended family workshops to learn social emotional development practices since 2016. Learn more about the program and its impact here.
She just gets it done
Sarah Miles, Mental Health Training Coordinator
 Sarah Miles previously served as the Mental Health Training Coordinator for 1,600 public schools across New York City. In this role, she created foundational mental health presentations and trainings for her sites and become known as a resource for staff, students and parents alike. When schools closed and students switched to digital learning for the first time in the City’s history, her office was inundated with more requests for help than they could have anticipated.
Sarah Miles previously served as the Mental Health Training Coordinator for 1,600 public schools across New York City. In this role, she created foundational mental health presentations and trainings for her sites and become known as a resource for staff, students and parents alike. When schools closed and students switched to digital learning for the first time in the City’s history, her office was inundated with more requests for help than they could have anticipated.
The needs varied. One family in Far Rockaway had a tech question about the iPad the Department of Education provided for their fifteen-year-old. Another family on the Lower East Side asked for support with self-care and stress management for their five-year-old. Committed to addressing these new needs, Sarah started to curate newsletters, webinars, and a wealth of other resources for parents, students, teachers, and mental health staff. She also helped school-based providers transition to tele-mental health services, providing critical care for students and families who were struggling with grief and loss.
Ms. Miles took extra care to make sure that everything she distributed was appropriate and relevant to the communities who were requesting help. Keeping in mind the City’s diverse population, Ms. Miles compiled resources for the LGBTQ+ community as well as resources specific to different ethnic groups and cultures, providing translated materials as much as she could.
“Sarah has a thoughtful, considerate, and respectful mind,” said Scott Bloom, Director of School Mental Health Services. “I often say Sarah, what do you have to offer? And Sarah just gets it done. She might be busy, but she’ll still say, ‘Oh, I can get that for you.’”
From Ms. Miles:
“I am drawn to working in children’s mental health because I see the need for reform and change in our systems and because I am passionate about being a positive connection and support for youth. My drive comes from the hope and possibility for change in individuals, communities, and systems – change is hard, but connection and relationships help me see where it’s possible.”
The Mayor’s Office of Community Mental Health program: Mental Health Services in High-Need Schools
The Mayor’s Office of Community Mental Health has also partnered with the Department of Education (DOE) to significantly enhance access to mental health support in New York City’s public schools. In Fiscal 2020, ThriveNYC partnered with DOE to offer onsite mental health support in high-need schools, including clinicians in 248 schools and access to onsite mental health clinics in 129 of those schools. Over 181,300 students have received individual and group counseling through this program since is launched in 2017. During the COVID-19 pandemic, students in high-need schools and students enrolled in school-based mental health clinics continued to receive therapy remotely. Learn more about the program and its impact here.
Taking on whatever challenge comes her way
Dr. Amber Testa, psychologist and the Clinical Supervisor for Communicable Disease Unit and North Infirmary Command
 As a clinical supervisor at the Rikers Island’s infirmary, Dr. Amber Testa’s main responsibility is primarily to oversee the staff of clinicians to provide some direct patient care. But when COVID-19 came to Rikers, that all changed. Dr. Testa found herself on the frontlines of an unprecedented crisis.
As a clinical supervisor at the Rikers Island’s infirmary, Dr. Amber Testa’s main responsibility is primarily to oversee the staff of clinicians to provide some direct patient care. But when COVID-19 came to Rikers, that all changed. Dr. Testa found herself on the frontlines of an unprecedented crisis.
The infirmary experienced a surge of patients needing care and attention, including patients with serious mental illness who were struggling with high levels of fear and anxiety as they waited for COVID-19 test results or were isolating after possible exposure.
Through all of this stress and uncertainty, patients and staff looked to Dr. Testa as a constant source of reassurance. She took on all challenges that came her way, whether it was in her job description or not.
“I have an image of Dr. Testa in full PPE going from one housing area to another, meeting with patients and checking in with them constantly,” said Dr. Virginia Barber-Rioja, Co-Chief of Mental Health for NYC Health + Hospitals/Correctional Health Services. “She was doing direct care, more than what was expected of her, and she was always willing to help. For a couple of days, she couldn’t come to work because she was sick, but even then, she was still calling the jail to check in with her staff and patients.”
From Dr. Testa:
“Psychology has been my passion for 15 years and shifting to work in a correctional setting with some of New York’s most underserved populations was a life-changing moment for me. It’s a continuous learning process and while it can be challenging, I show up for work for our patients, many of whom may feel abandoned by society or suffer alone in silence. I come to work for my incredible multidisciplinary team — mental health, medical, nursing, all the Correctional Health Services support services, our partners at the Department of Correction — who are all brave, dedicated and supportive individuals. I witness their daily heroism and come in to fight alongside them to protect and help our patients as best as we can.”
Related Mayor’s Office of Community Mental Health program: Behavioral Health Assessment and Support for Youth in Detention
Correctional Health Services (CHS) offers behavioral health screening, substance use engagement, and therapeutic creative arts programming for all young adults incarcerated in City jails and detention facilities. Since launching in 2016, this program has screened over 1,400 youth and young adults for behavioral health needs and provided over 5,500 creative arts therapy sessions in City jails and detention facilities. Learn more about the program and its impact here.
Offering a lifeline to sick patients when they needed it most
Jodi Romano, the Director of Mental Health Services at NYC Health + Hospitals/Elmhurst Hospital
 Being a hero sometimes means overcoming one’s fear in order to do what’s right. For Jodi Romano, the Director of Mental Health Services at Elmhurst Hospital, overcoming her fear during the coronavirus pandemic meant that countless sick patients were able to connect with their loved ones during one of the most challenging moments of their lives.
Being a hero sometimes means overcoming one’s fear in order to do what’s right. For Jodi Romano, the Director of Mental Health Services at Elmhurst Hospital, overcoming her fear during the coronavirus pandemic meant that countless sick patients were able to connect with their loved ones during one of the most challenging moments of their lives.
At the peak of the pandemic in March and April, Elmhurst Hospital saw a surge of COVID-19 patients. For healthcare workers like Ms. Romano in hard-hit hospitals across the City, the possibility of becoming sick with a dangerous and little-understood illness was a risk unlike any before. The risks were so great that hospital patients with COVID-19 were prohibited from seeing their loved ones in person. That left them without any outside support through a terrifying ordeal.
When Ms. Romano thought about how scared and alone those patients must have felt, she knew she had to put her own fears aside. Donning her PPE, she went into the hot zones of the hospitals, where there were the most COVID-19 patients, and brought along iPads to show patients how to connect remotely with their families and friends. She offered a lifeline to patients when they needed it most.
“Jodi helped patients overcome barriers, and that’s what social work is about,” said Charles Barron, Deputy Chief Medical Officer at H+H’s Office of Behavioral Health. “Seeing their families was very important to patients, and for Jodi, the patient comes first. She’s someone who really believes and cares.”
Now, because of Jodi’s efforts, the hospital has instituted an ongoing practice of helping patients get in touch with their loved ones.
“Jodi has always led by example,” Dr. Barron said. “This crisis showed her leadership and her willingness to take risks.”
From Ms. Romano:
“It is so important to me to treat our patients and their families the way I would want my family to be treated. I have the best job in the world. I get to help people live stronger and healthier lives. It is an honor to be part of their healthcare journey.”
Related Mayor’s Office of Community Mental Health program: Mental Health Service Corps
Elmhurst Hospital is one of the sites of the Mental Health Service Corps, a workforce development program that aims to build a diverse generation of mental health clinicians, equipped to integrate behavioral health into a variety of settings including primary care, women’s health, pediatrics, and other non-behavioral health care settings. Early-career clinicians receive intensive training in evidence-based practices and are placed throughout the NYC Health + Hospitals system with the goal of emerging from the three-year program seasoned and adept clinicians. Under the supervision of licensed clinicians, this intensive and innovative training experience will allow Corps Members to work effectively within interdisciplinary teams and prepared to screen, assess, and treat patients in a culturally competent manner. During the COVID-19 pandemic, Corps Members continued to deliver in-person and remote mental health services. Learn more about the program and its impact here.
Jumping in without hesitation
Dr. Roseann Titcombe-Parekh, Supervising Psychiatrist at Rikers Island
When Dr. Roseann Titcombe-Parekh was hired as a psychiatrist at the Rikers Island infirmary in February, she had no idea that within weeks she’d be facing an unprecedented public health crisis. Or that the crisis would dramatically change the nature of her role.
As the supervising psychiatrist for people with both serious mental illness and chronic medical conditions housed in the infirmary, Dr. Titcombe-Parekh was initially hired to work in a specialty housing area with individuals at elevated medical and mental health risk, and to provide support to other psychiatric providers in North Infirmary Command – but that job description quickly evolved.
As the coronavirus hit its peak in March and April, the needs of the patients and scope of the mental health service changed dramatically, and Dr. Titcombe-Parekh quickly adapted. She was reassigned from the infirmary to West Facility, where she began providing care to people diagnosed with COVID-19 who were developing a range of mental health problems. Roseann’s flexibility and courage was a source of inspiration for her team.
“We didn’t have a template or roadmap for handling COVID-19 and we didn’t know what to expect from our patients,” said Dr. Bipin Subedi, Co-Chief of Mental Health for NYC Health + Hospitals/Correctional Health Services.
“People could have had a lot of fear about working with patients who are COVID-19-positive, but not Roseann,” said Dr. Subedi. “She focused her energy on what she could do rather than what she was worried about. Even as a new hire and at a time of uncertainty, she jumped to help without any hesitation, taking responsibility for her patients and our mission to care for them.”
From Dr. Titcombe-Parekh:
“I was drawn to work in correctional psychiatry by the unique challenges and opportunities it presents. In treating our patients, we have the privilege of truly seeing, hearing, and caring for some of the most underserved and easily overlooked people in our community – this is important and fulfilling. I have an interest in understanding and treating trauma; something extremely pervasive in correctional health yet too frequently overlooked, under-appreciated, and inappropriately normalized. It is gratifying being able to treat our patients thoughtfully with the high standards of psychiatric medicine I was trained to provide, and with the humanity they deserve but so often do not receive. Though challenging at times, I am honored to commit myself to this work and humbled in doing so. I am incredibly grateful to have a team of like-minded, passionate, caring, and intelligent people to work with, who I continue to learn from.”
Related Mayor’s Office of Community Mental Health program: Behavioral Health Assessment and Support for Youth in Detention
Correctional Health Services (CHS) offers behavioral health screening, substance use engagement, and therapeutic creative arts programming for all young adults incarcerated in City jails and detention facilities. Since launching in 2016, this program has screened over 1,400 youth and young adults for behavioral health needs and provided over 5,500 creative arts therapy sessions in City jails and detention facilities. Learn more about the program and its impact here.
Making video therapy work for moms and young children
Tzivy Reiter, OHEL Children’s Home and Family Services, Brooklyn Early Childhood Therapeutic Center / Gladys Cortez-Feliciano, OHEL Children’s Home and Family Services, Brooklyn Early Childhood Therapeutic Center

When the COVID-19 pandemic first emerged in New York City and schools were forced to close their doors, Tzivy Reiter and Gladys Cortez-Feliciano understood that families with young children would need more support than ever. As clinicians at the OHEL Children’s Home and Family Services, part of the City’s Early Childhood Mental Health Network, they helped initiate the transition to tele-mental health at one of the network’s seven sites, making sure families felt comfortable joining video sessions and phone calls with clinicians.
Typically, OHEL serves mothers with infants and young children at their offices, but Ms. Reiter, who is Director of the Center, knew that without access to daycare centers and schools, mothers would be seeing them from their homes often surrounded by other children. Rather than ignore the distractions mothers now faced, she invited the whole family to participate in remote sessions. She developed a program—called the Pre-School Smile Club—that included all the children in a household up to six years old. The children sang, danced and were taught coping skills through movement and play. The model was so successful that they shared it with the rest of the Early Childhood Mental Health Network to invite the children from their agencies to participate. OHEL also shared best practices in engaging children and families, in a set of tele-mental health guidelines.
Reiter, who is Director of the Center, knew that without access to daycare centers and schools, mothers would be seeing them from their homes often surrounded by other children. Rather than ignore the distractions mothers now faced, she invited the whole family to participate in remote sessions. She developed a program—called the Pre-School Smile Club—that included all the children in a household up to six years old. The children sang, danced and were taught coping skills through movement and play. The model was so successful that they shared it with the rest of the Early Childhood Mental Health Network to invite the children from their agencies to participate. OHEL also shared best practices in engaging children and families, in a set of tele-mental health guidelines.
Ms. Cortez- Feliciano, a mental health consultant and clinician at OHEL, led the creation of several workshops for parents in English and Spanish. The workshops, conducted live on Zoom and recorded to share with the other families, helped parents cope with the new challenges they were facing, like teaching from home or self-care. This led Ms. Cortez-Feliciano to provide counseling for families to meet their individual needs.
Together, Ms. Reiter and Ms. Cortez-Feliciano make a dream team at OHEL. “Tzivy’s innovation is pretty remarkable,” said Fatima Kadik, Project Director for Early Childhood Mental Health Services. “And Gladys is willing to do so much—she’s an advocate for everyone.”
From Ms. Reiter:
“This work is very intense and difficult, but also very powerful. We see how the survivors find the strength within themselves to confront the deepest pain and move forward. It is humbling. It gives perspective on what truly matters, and inspires us to continue our work.”
From Ms. Cortez-Feliciano:
“It is important that the children and families I work with feel connected culturally and feel understood in their own language. I believe my work helps create a voice and empowers families as they grow through our working relationship. This could mean listening, creating awareness and developing insight, or getting their basic needs met, as well as connecting parents and children through art and play. This is how I strengthen the family’s toolbox to cope in the current crisis.”
The Mayor’s Office of Community Mental Health program: Early Childhood Mental Health Network
The Early Childhood Mental Health Network provides mental health support for young children and their families, helping to address challenges early. Seven early childhood therapeutic centers, open to all New York residents, located throughout the city offer specialized mental health treatment for children from birth to age five and their families, as well as access to family peer advocates and connection to ongoing support. Additionally, mental health professionals are able to receive specialized training in evidence-based practices and early childhood development through the Early Childhood Mental Health Training and Technical Assistance Center in order to increase the capacity and competencies of professionals working to identify and address the mental health needs of young children. Learn more about the program and its impact here.
Listening, not rushing in
Laura Dee and Mia Roberts, Early Childhood Social Workers, Brooklyn
Two Early Childhood Social Workers in Brooklyn have been doing all they can to help New Yorkers during the coronavirus pandemic, including shifting from supporting teachers and leaders at their school sites to providing remote support and sharing resources to help families and staff manage grief, loss, and trauma.
When schools closed and Laura Dee saw that families were losing loved ones, she knew her experience working in hospice could help. She used her expertise to help her Social Worker colleagues understand how to best support people who are grieving.
“Laura has helped us understand how to listen and not rush in. Social workers tend to have a ‘righting reflex,’ meaning they want to have an answer right away,” said Virginia Cortes, Mental Health and Wellness Administrator. “But Laura showed us how to really sit with a person who’s suffering – to give someone the freedom to express what’s happening – as uncomfortable as that is.”
 During the pandemic, Ms. Roberts remained a steadfast support for families, offering a listening ear to even the most difficult stories. “She is someone who will say to you, ‘you can put it all here, and it’s okay,” said Ms. Cortes.
During the pandemic, Ms. Roberts remained a steadfast support for families, offering a listening ear to even the most difficult stories. “She is someone who will say to you, ‘you can put it all here, and it’s okay,” said Ms. Cortes.
Together, Ms. Dee and Ms. Roberts helped many families in Brooklyn cope during the difficult months of the pandemic.
“During COVID-19, our Social Workers have supported with such humanity, such heart, such emotion,” Cortes said. “They keep saying, what can I do to help?”
From Ms. Roberts:
“I have always been drawn to social work because I enjoy working closely with people to support them in discovering new and innovative ways to resolve or cope with life challenges. The resilience in others is what keeps me going.”
From Ms. Dee:
“Being a social worker allows me the unique privilege of hearing other people’s stories and provides me with the opportunity to support individuals, children/families and systems in achieving their goals. My belief that everyone needs someone on their side and that one person can truly make a difference is what keeps me going.”
The Mayor’s Office of Community Mental Health program: Social Emotional Learning
Social, emotional, and behavioral regulation skills are foundational for learning and well-being. Through a partnership between The Mayor’s Office of Community Mental Health and the Department of Education, Pre-K and 3-K programs across New York City provide social-emotional learning support to students, families, program leaders and teaching teams. Over 3,000 schoolteachers or program staff participated in at least one professional learning through this program since the program launched in 2016. And, an additional 3,000 parents and caregivers have attended family workshops to learn social emotional development practices since 2016. Learn more about the program and its impact here.
Doing her part to help each New Yorker get a fair shot
Cora Caputo, Early Childhood Social Worker in Queens
 As an Early Childhood Social Worker at the Department of Education, Cora Caputo is always there for New York City’s littlest learners. She makes sure the three and four-year olds in her care have nurturing places to learn and play, and the skills to express their needs and feelings in a healthy way.
As an Early Childhood Social Worker at the Department of Education, Cora Caputo is always there for New York City’s littlest learners. She makes sure the three and four-year olds in her care have nurturing places to learn and play, and the skills to express their needs and feelings in a healthy way.
When the COVID-19 outbreak began and classrooms shifted to remote learning, Ms. Caputo’s job became much harder to do – but more important than ever. She serves about 342 children across nine Pre-K sites in Elmhurst and Ridgewood, two neighborhoods in Queens that were particularly hard-hit by COVID-19. It was clear that her students and their families were in great need.
Ms. Caputo noticed in her virtual classrooms that families were struggling to provide some basic learning supplies at home – like the crayons and paints that help children tap into their creativity and communicate their feelings. So the problem-solving social worker sprang into action.
She began contacting several art supply companies until she received a large donation of crayons, markers, and paints. While the rest of the city was social-distancing, Ms. Caputo put on her mask and gloves and began packaging and delivering supplies to the sites that could distribute them to the families she serves.
“Cora has a heart of gold,” said Melanie Lawrence, Mental Health Wellness Administrator at the Department of Education. “We found out on a Sunday that we were shifting to remote learning and ever since that following Monday, she’s been nonstop trying to do her best for children and families. She took initiative and she had compassion. She’s just a wonderful person.”
From Ms. Caputo:
“Working with our youngest learners and families is my way of helping each New Yorker get a fair shot, and I get to work with the wonderful people that make up our Division of Early Childhood Education team.”
The Mayor’s Office of Community Mental Health program: Social Emotional Learning
Social, emotional, and behavioral regulation skills are foundational for learning and well-being. Through a partnership between The Mayor’s Office of Community Mental Health and the Department of Education, Pre-K and 3-K programs across New York City provide social-emotional learning support to students, families, program leaders and teaching teams. Over 3,000 schoolteachers or program staff participated in at least one professional learning through this program since the program launched in 2016. And, an additional 3,000 parents and caregivers have attended family workshops to learn social emotional development practices since 2016. Learn more about the program and its impact here.
Giving their all, even during a pandemic
Darlene Sierra and Vanessa Torres, Early Childhood Social Workers, Staten Island
Two Staten Island Early Childhood Social Workers, Darlene Sierra and Vanessa Torres, have gone above and beyond to help students and families during the coronavirus pandemic.

As our schools and businesses closed their doors to stop the spread of coronavirus, Ms. Sierra knew that the families she supported were dealing with unprecedented challenges. There was extreme uncertainty and fear around the virus, and tremendous anxiety over job loss – many of the families she served had members out of work.
Ms. Sierra began sending emails to school leaders and site directors to see how she could help. When one site director informed her that an unemployed family was having trouble accessing food, Darlene spent the weekend connecting them to a food pantry.
“When someone is having a hard time, Darlene is the one to pick that person back up,” said Claremarie Bonafede, Mental Health and Wellness Administrator in Staten Island.
Ms. Torres is also committed to helping her students, regardless of the hurdles in her way. Some of Ms. Torres’ students were getting evaluated for special education services when the pandemic ground the process to a halt. She spent hours on the phone to help complete the process. Ms. Torres also created supportive, highly personalized videos to share resources directly with families—work she continued after she herself became sick with coronavirus. Ms. Torres also gave support to a Spanish-speaking family who had no computer access and limited ability to communicate with their school.
“These two are highly motivated and always want to make a difference in people’s lives,” said Claremarie Bonafede. “They’ve both given their all during this time, even through sickness.”
From Ms. Sierra:
“I was drawn to be a Social Worker since watching children grow is what I look forward to everyday. Helping parents be the best they can be is what I continue to do. It is truly an honor being able to touch people’s lives in different ways.”
From Ms. Torres:
“The ability to witness the journey of a young learner has been the motivating factor of my work. The glimmer of a child’s eye during this experience is unforgettable.”
The Mayor’s Office of Community Mental Health program: Social Emotional Learning
Social, emotional, and behavioral regulation skills are foundational for learning and well-being. Through a partnership between The Mayor’s Office of Community Mental Health and the Department of Education, Pre-K and 3-K programs across New York City provide social-emotional learning support to students, families, program leaders and teaching teams. Over 3,000 schoolteachers or program staff participated in at least one professional learning through this program since the program launched in 2016. And, an additional 3,000 parents and caregivers have attended family workshops to learn social emotional development practices since 2016. Learn more about the program and its impact here.
Helping employers manage uncertainty and promote workplace mental health
Dr. Nicole Andreoli, Clinical Psychologist
 With years of experience as a clinical psychologist, when Dr. Nicole Andreoli saw the dire mental health implications of the COVID-19 pandemic, she wanted to help. When Thrive in Your Workplace reached out to her to help lead a training for employers and employees affected by the pandemic, Dr. Andreoli didn’t hesitate to say yes.
With years of experience as a clinical psychologist, when Dr. Nicole Andreoli saw the dire mental health implications of the COVID-19 pandemic, she wanted to help. When Thrive in Your Workplace reached out to her to help lead a training for employers and employees affected by the pandemic, Dr. Andreoli didn’t hesitate to say yes.
New Yorkers spend a significant amount of their lives working and Thrive in Your Workplace is designed to help workplaces become on-ramps to mental health care, increasing access to support for one in five New Yorkers who experience mental illness every year. During the COVID-19 pandemic, embedding mental health support into workplaces has been as important as ever. In a national poll conducted earlier this year, 85% of workers reported being “worried and anxious they may lose their jobs” and 84% reported “really struggling” with employment-related matters.
To create a training that would address the urgent needs of workers during the pandemic, Dr. Andreoli began by looking at the effect of COVID-19 on employee mental health. That included the stress faced by essential employees who were on the frontlines, the anxiety of employees who were working remotely for the first time, and how to manage uncertainty during this unprecedented moment in time.
The goals of the training were twofold: Thrive in Your Workplace wanted to teach employees how to reduce stress as well as train employers on how to promote mental health in the workplace. To this aim, Dr. Andreoli presented actionable coping techniques like how to identify and manage negative thought patterns and how to practice mindfulness, as well as guidance on how organizations could create new opportunities for support through peer programs, manager trainings and expanded benefits.
“We looked at existing trainings, but what was missing was how to manage uncertainty,” said Rachael Steimnitz, Senior Manager, Program Implementation, Mayor’s Office of Community Mental Health. “Dr. Andreoli did research, provided a whole host of resources, and helped us create a new curriculum that responded to the unprecedented realities many workers are facing during this pandemic.”
Now, that training is posted online for any employer looking for information on how to support employee mental health during the pandemic. The video has received hundreds of views. The key to Dr. Andreoli’s success, said Sophie Pauze, Director of Strategic Partnerships at ThriveNYC, is her ability to get through to people about a topic that is often stigmatized, and can feel complex or intimidating.
“Dr. Andreoli was just really eager to help,” said Ms. Pauze. “She has a lot of generosity of spirit.”
From Dr. Andreoli:
“It is so wonderful to be a part of someone’s therapeutic journey, and to have a glimpse into the most private parts of someone. It is such a rewarding experience to watch the therapeutic transformation and see someone walk away lighter and freer, or to see how they have grown as a result of sharpening their mental health skills, strengthening core values or engaging in self-discovery.”
The Mayor’s Office of Community Mental Health program: Thrive in Your Workplace
During the COVID-19 pandemic, Thrive in Your Workplace offered remote technical assistance and training to employers and employees to help them address mental health needs. This included the publication of the COVID-19 Mental Health Guide for Employers as well as ten new workplace mental health virtual trainings. Learn more about the program and its impact here.
Elevating work with data, seven days a week
Richard Gamarra, Data Analyst

Richard Gamarra is a data analyst in the Division of Mental Hygiene at the NYC Department of Health and Mental Hygiene (DOHMH). Mr. Gamarra’s role collecting and analyzing data rarely puts him in the limelight—but it is critical in understanding how to best address the mental health needs of New Yorkers.
As the pandemic raged through the city, staffing changes in his unit left Mr. Gamarra handling the jobs of three different programs, including Co-Response Teams, which include police officers and clinicians who proactively engage people with mental illness and substance use disorders who may be at an elevated risk of harm to themselves or others.
During the pandemic, these programs could no longer operate in person the way they once did – and that meant that the way Mr. Gamarra measured their effectiveness also had to change. He acted quickly to develop an alternative data entry system, without any model to guide his work.
That’s not the only time Mr. Gamarra stepped up. When the Department of Homeless Services began helping New Yorkers experiencing homelessness relocate to isolation hotels, Mr. Gamarra volunteered to provide daily data on how the new program was working. With this new undertaking on top of ongoing responsibilities, Mr. Gamarra was working seven days a week.
“Richard has an ‘I can do this’ attitude,” said Athea Long, Executive Director for Crisis Prevention and Intervention Unit in Bureau of Health Promotion for Justice-Impacted Populations, Division of Mental Hygiene at the Department of Mental Health and Hygiene. “He works very hard and he’s very humble, but the things he’s doing are tedious and take a lot of time and energy. But no matter what I ask, he says ‘I got you.’”
From Mr. Gamarra:
“A lot of my colleagues are doing great work around the city providing mental health services to vulnerable community members. I am motivated by my desire to elevate their work in the most effective and responsible manner possible so that it may continue.”
The Mayor’s Office of Community Mental Health program: Co-Response Teams
Co-Response Teams, a collaboration between the New York City Police Department (NYPD) and the Department of Health and Mental Hygiene (DOHMH), are a pre- and post-crisis intervention. In the last four years, Co-Response Teams have assisted over 1,900 people across the city. Each team includes two police officers and one behavioral health professional from DOHMH. Teams are available 16 hours a day, seven days a week to assist people with mental illness and substance use disorders who may be at an elevated risk of harm to themselves or others. Co-Response Teams connect or re-connect community members to care or another stabilizing support, including medical, mental health, legal, housing and other social and clinical services. These teams aim to reduce the number of enforcement interactions with the Police Department and create greater stability for these New Yorkers. During the COVID-19 pandemic, Co-Response Teams engaged people and their support network (such as family members, service providers, and friends) by phone 4,470 times. Learn more about the program and its impact here.
Making sure frontline mental health workers have the support they need
Yan Mei Nie, Quality Improvement Specialist at NYC Well
 Yan Mei Nie is a rising star on the NYC Well team. Hired in February 2019 as a counselor to respond to calls, texts, and chats to the City’s comprehensive mental health helpline, she was quickly promoted to Quality Improvement Specialist, right as the coronavirus pandemic began.
Yan Mei Nie is a rising star on the NYC Well team. Hired in February 2019 as a counselor to respond to calls, texts, and chats to the City’s comprehensive mental health helpline, she was quickly promoted to Quality Improvement Specialist, right as the coronavirus pandemic began.
Part of a Quality Improvement Specialist’s role is to give feedback to NYC counselors so they can deliver the highest quality support to New Yorkers seeking help. For many people, this can be an uncomfortable role since it means critiquing a counselor’s work and offering suggestions for improvement. But it’s a role that Ms. Nie excels at. Her empathetic nature, and the fact that she started as a Counselor on the NYC Well team, means that her feedback is always well-received.
As calls to NYC Well increased during the pandemic, Ms. Nie became all the more supportive of her team. She understood that many members of the counseling team were experiencing their own mental health challenges in response to the pandemic, even as they responded to thousands of New Yorkers who were struggling.
So, she took it upon herself to improve the morale and wellbeing of staff. She became active in a wellness committee to address NYC Well counselors’ mental health needs. She also began searching for professional development opportunities that could help her colleagues address short-term and long-term challenges related to COVID-19. Ms. Nie knew that preparing counselors to handle the influx of COVID-19-related calls would help them reduce their stress and continue to provide a consistently high level of care to New Yorkers.
“Yan Mei Nie is extremely professional and really driven to provide a high level of service,” said Kelly Clarke, Program Director of NYC Well. “She shows up that way in every setting – in team meetings, and in the way she engages with management and colleagues. She always creates a nonjudgmental space.”
From Ms. Nie:
“What drew me to work in this field was the incredible opportunity to provide emotional support for people going through a crisis. I am proud to be a part of an organization that is strongly dedicated to making a positive impact on mental health.”
The Mayor’s Office of Community Mental Health program: NYC Well
NYC Well provides a single point of entry to the City’s mental health and substance misuse services via comprehensive 24/7/365 support over the phone, through text messaging, or through online chat. NYC Well provides robust crisis counseling, referrals to ongoing care, help with scheduling appointments, connection to mobile crisis services, peer support, and follow-up. NYC Well works to connect people to appropriate services regardless of insurance or immigration status. During the COVID-19 pandemic, NYC Well responded to an increased need. NYC Well answered 17% more calls in May 2020 than in May 2019, and more calls in June 2020 than in June 2019. There were more than 120,000 visits to the NYC Well website in April 2020 – up 400% from April 2019. Any New Yorker in need – or who knows someone in need – can call 888-NYC-WELL (1-888-692-9355), text WELL to 65173, or chat online at nyc.gov/nycwell. Learn more about the program and its impact here.
Bringing medication to people in their communities
Dr. Lance Winslow, Mobile Crisis Director at Kings County Hospital
 Every day for seven years, Dr. Lance Winslow has made the hours-long commute from his home to Kings County Hospital in Central Brooklyn. At the hospital, Dr. Winslow is known for always serving members of the community with a smile on his face – even though his job leading a Mobile Crisis Team is a stressful one, pandemic or not.
Every day for seven years, Dr. Lance Winslow has made the hours-long commute from his home to Kings County Hospital in Central Brooklyn. At the hospital, Dr. Winslow is known for always serving members of the community with a smile on his face – even though his job leading a Mobile Crisis Team is a stressful one, pandemic or not.
Dispatched via NYC Well or NYC Health + Hospital facilities, Mobile Crisis Teams typically provide in-person services to people with an urgent mental health problem. While medical staff in traditional clinical settings have access to a number of supports – like detailed medical histories – Mobile Crisis Teams often arrive at a home with limited information, sometimes only an address and phone number.
With the onset of the COVID-19 pandemic, hospital psychiatric staff noticed that some of their patients with serious mental illness were missing their appointments, leaving them without the medication they need to manage symptoms. The number of patients who regularly came in to receive long-acting injections at the Kings County Outpatient Center dropped dramatically.
That’s when Dr. Winslow stepped up. He saw an opportunity for Mobile Crisis Teams to reach the New Yorkers who couldn’t safely come to the outpatient clinic.
Dr. Winslow and his team began traveling to people’s homes to administer their psychiatric medications, in addition to the normal functions his team provides on a daily basis. It was the first time Mobile Crisis Teams proactively delivered medication and support to patients outside of the NYC Well referral system.
“We had never done this before,” said Dr. Renuka Ananthamoorthy, Chief of Behavioral Health Services at NYC Health + Hospitals/Kings County Hospital. “But Dr. Winslow is innovative and passionate about his work, and now even more so during the coronavirus outbreak. He came to work every day and said all he needed was a mask, glove, and hand sanitizer. As long as he had those three things, he would go see his patients.”
From Dr. Winslow:
“I look forward to my work due to the amazing potential to change and impact lives each and every day. Going out into the community to assess, support and brainstorm solutions with our consumers who face a variety of challenges, is not only the most exciting profession, but the most rewarding job available.”
The Mayor’s Office of Community Mental Health program: NYC Well and Mobile Crisis Teams
NYC Well, the City’s comprehensive mental health helpline and a signature Mayor’s Office of Community Mental Health program, deploys Mobile Crisis Teams operated by hospitals and community-based organizations to respond to urgent mental health needs. Deployed approximately 21,000 times per year, Mobile Crisis Teams often serve children and adults in their homes. Mobile Crisis Teams can include nurses, social workers, psychologists and psychiatrists, community liaisons and peers. Teams can arrive within hours of a referral and services can include assessment, crisis counseling, and connection to ongoing services. Learn more about the program and its impact here.
When she speaks, everyone listens
Lisa Lerner, Psychotherapist, Manhattan Family Justice Center
 Lisa Lerner often leads the way at the Manhattan Family Justice Center (FJC), which helps survivors of domestic and gender-based violence find their way to safety and healing.
Lisa Lerner often leads the way at the Manhattan Family Justice Center (FJC), which helps survivors of domestic and gender-based violence find their way to safety and healing.
An experienced psychotherapist, Ms. Lerner and her colleague, Dr. Gloria Ellis, brought an integrated psychotherapy and psychiatry mental health treatment model to the Manhattan FJC for the first time. She then trained social service and legal staff in simple ways to support clients who may have mental health challenges.
Lisa also created a support group for the Manhattan FJC’s legal counselors, to help them cope with a phenomenon called vicarious trauma. This occurs when frontline client-facing staff are profoundly affected by the trauma in their clients’ lives. Staff say the group helped bring a cohesive nature to their work environment.
When the coronavirus pandemic hit, Ms. Lerner once again pioneered a new approach, spearheading the Manhattan FJC’s effort to provide remote support for survivors of violence.
At first, the FJC team was unsure that an online support group would work—it was daunting to manage a sensitive topic online, especially since it can be difficult to gauge emotions when you can’t see group members in person to fully appreciate their body language.
“There are a lot of hurdles to providing healthcare remotely, and you have to be thoughtful and creative,” said Dr. Obianuju Berry, incoming Medical Director of the NYC Gender-Based Violence Mental Health Collaboration at NYC Health + Hospitals/NYU. “But Lisa led the way in taking on this new medium.”
Thanks to Ms. Lerner’s work, the group went off without a hitch. Survivors enthusiastically participated and were able to open up, and the Manhattan FJC continues to hold the sessions online. And the staff continue to look to Ms. Lerner as a leader.
“She’s soft-spoken, but when she speaks everyone really listens,” said Dr. Elizabeth Murphy Fitelson, Director of the Women’s Program in Psychiatry at Columbia University, which has been collaborating on this project since 2013. “All of us admire her a great deal.”
From Ms. Lerner:
“Being the descendant of survivors of persecution, I find that my work with survivors of intimate partner violence helps keep me connected to my own ancestors’ resilience. I feel privileged to bear witness to my clients’ experiences, and humbled to play a part towards their healing journey.”
The Mayor’s Office of Community Mental Health program: Mental Health Services in Family Justice Centers (FJCs)
To bring mental health support to survivors of intimate partner violence, the Mayor’s Office of Community Mental Health partners with the Mayor’s Office to End Domestic and Gender-Based Violence and NYC Health + Hospitals to add dedicated mental health teams to Family Justice Centers (FJCs). These new mental health teams include a full-time therapist, a part-time psychiatrist, and a full-time program administrator who provide direct on-site clinical services and complement the trauma-informed, comprehensive services available in each of the City’s five FJCs. Over 1,060 clients have been served by this program since the program launched in 2016, many of whom attended multiple clinical sessions. Learn more about the program and its impact here.
Making sure no one falls through the cracks
Yolanda McCray, Crime Victim/Domestic Violence Advocate at 28th Precinct in Central Harlem
 Yolanda McCray has been a Crime Victim/Domestic Violence Advocate in the 28th Precinct in Central Harlem since 2017. As a victim advocate, she reaches out to people who have filed police reports to offer her support, help them navigate the criminal justice process, and advocate for whatever they need – from social services to new housing, to court orders of protection.
Yolanda McCray has been a Crime Victim/Domestic Violence Advocate in the 28th Precinct in Central Harlem since 2017. As a victim advocate, she reaches out to people who have filed police reports to offer her support, help them navigate the criminal justice process, and advocate for whatever they need – from social services to new housing, to court orders of protection.
Ms. McCray has strong connections to her community and at the precinct where she works. She’s gained a reputation for constantly building and strengthening relationships with community organizations that can help her clients.
That’s why, when Ms. McCray and her team had to work remotely to stop the spread of COVID-19, police officers in the precinct often called her to make referrals for clients that needed support. “It wasn’t just one or two referrals, it was all of them,” said Liliana Peralta, Manager at the Crime Victim Assistance Program/Safe Horizon.
Ms. McCray’s clients know they can always reach her.
“When you walk down the street with Yolanda, people know her. They say, ‘Hey Ms. McCray.’ She really cares about the community,” said Peralta. “One of her favorite phrases is, ‘I don’t want this person to fall through the cracks.’ That’s something she says all the time. I’m so thankful for people like Yolanda.”
From Ms. McCray:
“Advocacy supports a voice to those who feel invisible. My motivation supports empowerment to those who are classified as underserved. My clients are my heroes, they show me that with patience, empathy and a helping hand, what is possible to achieve.”
The Mayor’s Office of Community Mental Health program: Crime Victim Assistance Program
Before the Mayor’s Office of Community Mental Health, many crime victims navigated the complicated landscape of the criminal justice and social service systems alone. Just three precincts had one onsite victim advocate to serve victims of domestic violence. Now, victims of any kind of crime can be served by the Crime Victim Assistance Program, which operates in precincts and Housing Police Service Areas citywide and has served over 165,000 people since 2016. The program provides supportive counseling, connections to individual or group therapy, safety planning, assistance with victim compensation, and help navigating the legal and financial challenges that can emerge after a crime has occurred. During the COVID-19 pandemic, victim advocates provided remote support to people harmed by crime, violence or abuse. Learn more about the program and its impact here.
Helping students have difficult conversations about loss
Miriam Berman, School Response Clinician
 During the COVID-19 pandemic, Miriam Berman has had to reimagine her work as a School Response Clinician (SRC) at New York City public schools. Usually, SRCs provide care for students in times of immediate crisis or emotional distress by providing onsite clinical counseling and connecting students to long-term care. But when the schools shifted to remote learning, that in-person support was impossible to provide.
During the COVID-19 pandemic, Miriam Berman has had to reimagine her work as a School Response Clinician (SRC) at New York City public schools. Usually, SRCs provide care for students in times of immediate crisis or emotional distress by providing onsite clinical counseling and connecting students to long-term care. But when the schools shifted to remote learning, that in-person support was impossible to provide.
Instead of slowing down, Ms. Berman jumped into action. The bulk of Ms. Berman’s remote work with schools involved providing counseling for students who had lost a family member due to COVID-19. She created and ran virtual support groups for staff across many schools.
Ms. Berman also helped develop an easily accessible Google Classroom to connect families to essential resources like food, internet, and tele-mental health services. She began conducting remote counseling sessions to support students and families who were struggling with the ongoing crisis as well as those who were grieving the loss of a relative due to COVID-19.
Knowing that entire school communities were experiencing trauma, Ms. Berman began running virtual support groups and social-emotional learning sessions for teachers and administrators on how to support a whole school – students, families and staff included – during a pandemic. She also created a COVID-19 loss referral form with guiding language so that teachers who were having difficult conversations about grief with students could refer them to an SRC for additional support.
“Navigating relationships virtually can be hard,” said Carmen Villavicencio-Hein, Supervisor of School Social Workers. “Miriam needed to really work on how to allocate supports throughout schools, and also how we would deploy them in a virtual world.”
During the pandemic, Ms. Berman also volunteered to work at the City’s Regional Enrichment Centers for children of essential workers, many of whom were first responders and other key personnel leading the City’s fight against COVID-19. There, she provided student support and implemented a social and emotional curriculum, to help children identify and cope with their feelings while navigating all the new transitions. Ms. Berman knew that first responders needed space to process their own experiences and possible trauma, so she volunteered to co-facilitate groups to support nurses.
“What Miriam did, volunteering and managing the demands of her own position, was huge. She balanced all those things,” said Ms. Villavicencio-Hein.
From Ms. Berman:
“Empowering children with confidence and skills to navigate life’s challenges led me to this work and I’m continuously inspired by the strength and resiliency of our students and families. It’s beautiful to see people come together to support each other through times of crisis.”
The Mayor’s Office of Community Mental Health program: School Response Clinicians
In the beginning of the 2019/2020 school year, the City launched a new partnership between the Mayor’s Office of Community Mental Health and DOE: School Response Clinicians, licensed clinical social workers who support students across the city. These social workers provide care to students to prevent crises and in times of immediate emotional distress, provide onsite counseling, and help connect students to long-term care if necessary. During the COVID-19 pandemic, School Response Clinicians offered wellness check-in calls and individual mental health sessions remotely to students in emotional distress or crisis. Learn more about the program and its impact here.
She doesn’t wait to begin helping survivors
Iris Wong, Domestic Violence Advocate, Crime Victim Assistance Program

At the precinct she serves in Queens, you might see Iris Wong in the waiting room, offering her assistance – or a hot cup of coffee – to fellow Cantonese speakers. Ms. Wong is a committed Domestic Violence Advocate with the Crime Victim Assistance Program (CVAP). She is an invaluable resource for survivors of violence in the community, especially for Chinese and Chinese-American New Yorkers.
Typically, advocates get in touch with clients after a referral from an officer, but Ms. Wong often doesn’t wait. She can be found checking the waiting room or posting Cantonese flyers with her contact information wherever survivors might see them.
Ms. Wong’s go-getter spirit became even more evident during the pandemic, when many of her clients faced new challenges and dangers while staying at home. In addition to an ongoing domestic violence situation, one client was anxious about losing his job, and struggling with teaching his daughter from home. Ms. Wong was available around the clock to assist him.
After Ms. Wong spent her day off assisting this client, he asked to speak directly to her supervisor—just so that he could sing Ms. Wong’s praises. “I’ve worked with many government workers,” said the client, “but none of them have really cared like Iris.”
According to Lizette Felipe, Manager at Safe Horizon, the non-profit that implements the Crime Victim Assistance Program, that’s not an uncommon experience. “I’ve gotten calls and emails about how well Iris has done,” Ms. Felipe said. “It’s because she listens genuinely—Iris doesn’t have a checklist or a script. Everything comes from her heart.”
From Ms. Wong:
“I do this work because I know there are many individuals in the Asian community who are underserved due to language barrier and lack of representation. I want to help all individuals achieve their best possible levels of personal and social well-being.”
The Mayor’s Office of Community Mental Health program: Crime Victim Assistance Program
Before the Mayor’s Office of Community Mental Health, many crime victims navigated the complicated landscape of the criminal justice and social service systems alone. Just three precincts had one onsite victim advocate to serve victims of domestic violence. Now, victims of any kind of crime can be served by the Crime Victim Assistance Program, which operates in precincts and Housing Police Service Areas citywide and has served over 165,000 people since 2016. The program provides supportive counseling, connections to individual or group therapy, safety planning, assistance with victim compensation, and help navigating the legal and financial challenges that can emerge after a crime has occurred. During the COVID-19 pandemic, victim advocates provided remote support to people harmed by crime, violence or abuse. Learn more about the program and its impact here.
Determined to make contact
Assertive Community Treatment (ACT) Team, Elmhurst Hospital
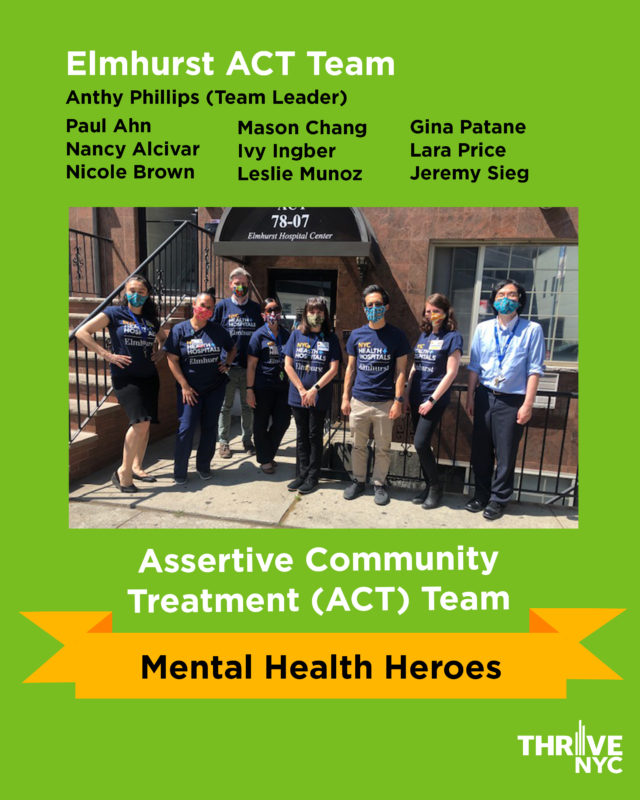 Assertive Community Treatment (ACT) teams go to great lengths to help New Yorkers with serious mental illness stay connected to treatment and remain in their own communities — whether that means meeting them in the park or in a building hallway. They bring mobile mental health treatment and medication to clients and connect them to services like food and housing when needed.
Assertive Community Treatment (ACT) teams go to great lengths to help New Yorkers with serious mental illness stay connected to treatment and remain in their own communities — whether that means meeting them in the park or in a building hallway. They bring mobile mental health treatment and medication to clients and connect them to services like food and housing when needed.
The ACT team based out of Elmhurst Hospital is used to going the extra mile to reach people in need. Because Queens is one of the most diverse places in the world, the team serves patients – and their families – from countries all across the globe. That’s why their small team has such out-sized language capacity, with speakers of English, Spanish, French, Mandarin and Korean. They know how important it is to make people feel comfortable and safe, especially for those worried about their immigration status.
With the transition to telehealth during the COVID-19 pandemic, the Elmhurst ACT Team suddenly faced new challenges. Some patients did not have the necessary technology or were hesitant to use it. Others were suddenly harder to find, and nearby shelters and nursing homes had less capacity to help locate them.
These tough logistical challenges were compounded by the emotional and physical devastation of the moment. The community they serve was one of the hardest hit by COVID – not just in the city, but in the entire country. The ACT Team saw their colleagues at the hospital and patients getting sick, and soon learned that two of their patients tragically passed away. Still, the ACT Team carried on, knowing their work was more important than ever.
They continued to deliver medication in the field, and applied safety precautions so they could accept walk-ins at their hospital office. And despite initial reservations from some patients, they met with patients by phone at least twice a week. When they couldn’t immediately locate a person, they searched until they found him or her. And when the team realized that a typically hard-to-locate patient in Queens needed a phone, they purchased one for him. Now this client has had more sessions with the team than ever before.
“This team was working in ground zero,” said Evelyn Barbosa, Senior Program Specialist, Health Services Manager, at the Department of Health and Mental Hygiene’s Treatment office. “They functioned at a level that was extraordinary for a team located in such a hard hit area. They never complained. They were determined to make contact with clients. They made sure people were not left out in the streets.”
From Anthy Phillips, Team Leader of Elmhurst ACT:
“Our Team is dedicated to providing quality care for individuals who are often overlooked or fall through the cracks of the mental health system. The team’s cohesion helped us through the pandemic and actually brought us closer. We were all in it together.”
The Mayor’s Office of Community Mental Health program: Assertive Community Treatment (ACT) Teams
Managed by the Department of Health and Mental Hygiene, Assertive Community Treatment (ACT) Teams include mental health and substance use professionals and, at times, peer specialists. ACT teams typically meet with clients six times per month in their home or community to provide long-term behavioral health treatment, including medication. The Mayor’s Office of Community Mental Health added a master’s level Substance Use Specialist to 40 ACT teams, enhancing these teams’ ability to serve people with co-occurring disorders. Treatment by ACT teams has led to reduced homelessness and fewer psychiatric hospitalizations among the people they serve. During the COVID-19 pandemic, ACT Teams provided a combination of tele-mental health and in-person services in order to successfully continue serving the same number of clients during the height of COVID-19 as they did before the pandemic. Learn more about the program and its impact here.
Unflagging optimism, even during a crisis
Salley May, Lead Social Worker, Mobile Crisis Unit
For 19 years, Salley May has been a valued member of the Mobile Crisis Team unit at Bellevue Hospital – she is the most experienced social worker on the team. Dispatched via NYC Well or NYC Health + Hospital facilities, Mobile Crisis Teams typically provide in-person services to people with an urgent mental health problem.
Convincing someone in crisis to receive help voluntarily takes an enormous amount of patience and skill. At the height of the COVID-19 pandemic, this was especially difficult. “Even in the best of times, it can be hard to persuade someone to work with you,” said Charles Barron, Deputy Chief Medical Officer at H+H’s Office of Behavioral Health. “Now to show up wearing PPE and trying to say ‘trust me’ during a health crisis, it seems like it’s doubly hard.”
But difficulty doesn’t deter Ms. May. When someone was reported for unsafe behavior in his neighborhood, Ms. May made repeated contacts with the person until she was able to build trust with him. Eventually, she and her mobile crisis partner convinced him to join them in a taxi to the emergency room, where the person received mental health services, treatment for a wound, and medication for high blood pressure. She has performed similar feats for countless patients over the years.
“Salley understands what it’s like to have a substance abuse problem or no money or job, and she’s remarkable at treating everyone with respect,” said Dr. Mary Anne Badaracco, Chief of Psychiatry at Bellevue. “She can engage with a range of people and tune in to with what they need. She just has unflagging optimism.”
From Ms. May:
“I went back to school specifically to work at Bellevue, for its history, the mission of all our NYC public hospitals, and the incredible constellation of people that we serve. I’ve been a line worker in Bellevue’s CPEP and on the Mobile Crisis Team for the past 19 years, with intensified demand during COVID-19 to manage crises in the field despite a patient’s usual supports being closed or operating ‘remotely.’ In cases requiring hospital transport we worked to avoid added trauma to the patient and the overwhelmed EMS/NYPD system by getting the patient to voluntarily travel with us by taxi, which we were able to manage in all but two cases. I share this honor with my brilliant Bellevue mobile crisis team members and with my family who supports my being on the frontline, wherever that expands to.”
The Mayor’s Office of Community Mental Health program: NYC Well and Mobile Crisis Teams
NYC Well, the City’s comprehensive mental health helpline and a signature Mayor’s Office of Community Mental Health program, deploys Mobile Crisis Teams operated by hospitals and community-based organizations to respond to urgent mental health needs. Deployed approximately 21,000 times per year, Mobile Crisis Teams often serve children and adults in their homes. Mobile Crisis Teams can include nurses, social workers, psychologists and psychiatrists, community liaisons and peers. Teams can arrive within hours of a referral and services can include assessment, crisis counseling, and connection to ongoing services. Learn more about the program and its impact here.
A catalyst for change
Crystal White, Domestic Violence Advocate at Housing Police Service Area 1
 Crystal White, who works with survivors of domestic violence as an advocate with the Crime Victim Assistance Program, knows that home is not a safe place for everyone. As many New Yorkers stayed home to prevent the spread of COVID-19, Ms. White remained committed to finding safety for New Yorkers experiencing domestic violence.
Crystal White, who works with survivors of domestic violence as an advocate with the Crime Victim Assistance Program, knows that home is not a safe place for everyone. As many New Yorkers stayed home to prevent the spread of COVID-19, Ms. White remained committed to finding safety for New Yorkers experiencing domestic violence.
At the height of the pandemic, one of Ms. White’s clients needed to move out of her apartment quickly because of violence—a challenge in the best of times, made harder because most businesses were operating remotely. But Ms. White wasn’t deterred. She helped purchase an air mattress for her client, contacted moving companies, and helped secure new housing through the New York City Housing Authority.
Ms. White’s work didn’t end there. When her client began experiencing traumatic flashbacks during the move, Crystal got on the phone with the movers and helped them de-escalate the situation. Eventually, the client was calm enough to help the movers as they worked.
Tina Logan, Manager at Safe Horizon, the non-profit that implements the Crime Victim Assistance Program, says that Ms. White’s support for her clients and her tireless work in moving requests up the chain of command make her a standout advocate. At the Housing Police Service Area where she works, she has a widely known reputation for diligence. As a result, police officers reach out to her without hesitation and refer survivors to her. “She doesn’t just do the minimum,” said Tina Logan. “She herself is part of the process. Where another person might get frustrated because they can’t get through to a service, Crystal will keep trying until she reaches someone. She is a catalyst for change.”
From Ms. White: “I truly enjoy what I do which is helping people. There is no exercise better for the heart than reaching down and lifting people up.”
The Mayor’s Office of Community Mental Health program: Crime Victim Assistance Program
Before the Mayor’s Office of Community Mental Health, many crime victims navigated the complicated landscape of the criminal justice and social service systems alone. Just three precincts had one onsite victim advocate to serve victims of domestic violence. Now, victims of any kind of crime can be served by the Crime Victim Assistance Program, which operates in precincts and Housing Police Service Areas citywide and has served over 165,000 people since 2016. The program provides supportive counseling, connections to individual or group therapy, safety planning, assistance with victim compensation, and help navigating the legal and financial challenges that can emerge after a crime has occurred. During the COVID-19 pandemic, victim advocates provided remote support to people harmed by crime, violence or abuse. Learn more about the program and its impact here.
On the frontlines of recovery
Orkideh Yazhari and Mariah Moore, Mental Health Service Corps
 One serves at a hospital in Queens. The other, at a clinic in Brooklyn. Both joined the Mental Health Service Corps to provide mental health care at high-need sites in New York City. And during the COVID-19 pandemic, Mariah Moore and Orkideh Yazhari each went above and beyond to deliver on that promise.
One serves at a hospital in Queens. The other, at a clinic in Brooklyn. Both joined the Mental Health Service Corps to provide mental health care at high-need sites in New York City. And during the COVID-19 pandemic, Mariah Moore and Orkideh Yazhari each went above and beyond to deliver on that promise.
Ms. Yazhari is primarily based in the Queens Hospital Comprehensive Psychiatric Emergency Program or Psychiatric Emergency Room. She also sometimes covers for the Queens Hospital Mobile Crisis Team, which responds to urgent mental health needs, often serving people in their homes. During the COVID-19 pandemic, many New Yorkers in need of urgent psychiatric care were diverted to Queens Hospital. “Our Psychiatric Emergency Room was really busy in a way that we never experienced it before,” said Ms. Yazhari. After becoming sick herself with COVID, Ms. Yazhari came back right away after her recovery period in order to ensure Queens Hospital had sufficient coverage. She volunteered to stay longer hours and cover different shifts at time when the Hospital was short on staff.
Her responsibilities at the hospital varied each day, and Ms. Yazhari adapted to different workflows and responsibilities with a grace and poise that impressed her colleagues. With many hospital workers afraid of becoming infected themselves, Ms. Yazhari became a constant source of reassurance and support.
“She really was able to be the calming voice in the room and brought people’s anxiety levels down,” said Melanie Sanchez, Director of Mental Health Service Corps.
 When much of the nursing staff at Ms. Moore’s East New York clinic was redeployed to work with COVID-19 patients, patients with chronic disease were left without their usual care. Although Ms. Moore typically didn’t work with those patients, she stepped in to meet the emerging needs.
When much of the nursing staff at Ms. Moore’s East New York clinic was redeployed to work with COVID-19 patients, patients with chronic disease were left without their usual care. Although Ms. Moore typically didn’t work with those patients, she stepped in to meet the emerging needs.
When one of her new patients was discharged while still too weak to meet his basic needs, Ms. Moore set him up with meal delivery – no easy task at a time when they were only accepting online applications, and the patient had no internet access. “Mariah was doing this work alone,” said Sanchez. “It was such a feat, and Mariah jumped hurdles.”
“Social workers and mental health professionals are going to be at the frontlines of the recovery,” added Sanchez. “They’re going above and beyond.”
From Ms. Moore:
“I entered social work because I sought to discover myself in acts of services to others. I continue in social work because I believe that access to quality education, excellent health care, and comprehensive mental health services are human rights for all people; not just entitlements we strip away in moments of political folly.”
From Ms. Yazhari:
“Thankfully, we at Queens Hospital got through the difficult time during the height of COVID and were able to provide some psychiatric services to the wider Queens population. I started serving with Mental Health Service Corps about two years ago as a behavioral social worker in a psychiatric emergency department. As an immigrant who was given the opportunity to starting a new life, receiving the support after leaving an oppressive country and trauma of war, and receiving higher education, I chose the social work profession to serve and give back to the community who made it all possible for me. It is certainly an honor to serve those in need of mental health through the Mayor’s Office of Community Mental Health which assists those who are have experienced trauma in their lives and are underserved.”
The Mayor’s Office of Community Mental Health program: Mental Health Service Corps
Mental Health Service Corps is a workforce development program that aims to build a diverse generation of mental health clinicians, equipped to integrate behavioral health into a variety of settings including primary care, women’s health, pediatrics, and other non-behavioral health care settings. Early-career clinicians receive intensive training in evidence-based practices and are placed throughout the NYC Health + Hospitals system with the goal of emerging from the three-year program seasoned and adept clinicians. Under the supervision of licensed clinicians, this intensive and innovative training experience will allow Corps Members to work effectively within interdisciplinary teams and prepared to screen, assess, and treat patients in a culturally competent manner. In Fiscal Year 2020, more than 2,700 New Yorkers have received clinical services from Corps Members at high-need locations. During the COVID-19 pandemic, Corps Members continued to deliver in-person and remote mental health services. Learn more about the program and its impact here.
A partner in the care process for vulnerable young people
Jason Manizza, Mental Health Coordinator, Mental Health Support at Runaway and Homeless Youth Residences and Drop-In Centers
 For the past five years, Jason Manizza has been meeting and providing mental health counseling for runaway and homeless youth in New York City. During the COVID-19 pandemic, Mr. Manizza was there for the young residents – offering positive, encouraging support during some of the most challenging moments of their lives.
For the past five years, Jason Manizza has been meeting and providing mental health counseling for runaway and homeless youth in New York City. During the COVID-19 pandemic, Mr. Manizza was there for the young residents – offering positive, encouraging support during some of the most challenging moments of their lives.
As mental health coordinator at two residences that serve female-identifying youth from ages 16-20, Mr. Manizza provides diagnostic and individualized counseling for residents—including mothers and pregnant residents. He also helps connect residents to health insurance and other needed community-based services.
Throughout the pandemic, Mr. Manizza continued to meet with residents regularly. And with the onslaught of COVID-19-related stress and anxiety, some clients were in need of frequent sessions. His colleagues say he was there for them, too.
“Jason never shows any type of discouragement,” said Andrew Luong, Program Director at The Children’s Village. “In addition to being a stable support for the youth, Jason also helps staff cope and he also helps us better serve residents.”
Throughout the COVID-19 pandemic, The Children’s Village continues to provide critical housing and supportive services for runaway and homeless youth, and Jason plays a big role in ensuring the space is welcoming and healing. “Jason is compassionate, kind, and an expert mental health practitioner. He reminds us that our work is to help every young person as partners in the care process,” added Mr. Luong.
From Mr. Manizza:
“I’m drawn to providing mental health services for youth because, in my mind, they are our society’s lifeblood. What keeps me going is a cemented value for the young women I serve. Women bring us all into the world and are our most important human resource; they deserve our very best effort towards promoting their ability to thrive.”
The Mayor’s Office of Community Mental Health program: Mental Health Services in Runaway and Homeless Youth Residences and Drop-In Centers
The Department of Youth and Community Development (DYCD) funds Runaway and Homeless Youth (RHY) Drop-in Centers, Crisis Services and Transitional Independent Living Residential Programs, which provide specialized services to vulnerable youth, including LGBTQ+ identifying youth. The Mayor’s Office of Community Mental Health partners with DYCD’s RHY programs to enhance mental health services offered to young people residing in more than 40 RHY residential programs and eight drop-in centers across all five boroughs. Over 2,600 young people were served by mental health professionals in Fiscal Year 2020, and more than 13,600 young people have been served through this program since 2016. During the COVID-19 pandemic, mental health support continued to be provided to youth both in-person and through new tele-mental health services at residential programs (which remained open and operational during the pandemic) and drop-in centers (which operated on a modified schedule). Learn more about the program and its impact here.
Always on call
Jailene Panarella, Senior Victim Advocate, Special Victims Division of the Crime Victim Assistance Program
 Jailene Panarella works with survivors of sexual violence and abuse in the Special Victims Division of the Crime Victim Assistance Program (CVAP). When Jailene’s caseload decreased during the COVID-19 pandemic, Ms. Panarella didn’t slow down—she went into overdrive to support survivors’ emerging needs.
Jailene Panarella works with survivors of sexual violence and abuse in the Special Victims Division of the Crime Victim Assistance Program (CVAP). When Jailene’s caseload decreased during the COVID-19 pandemic, Ms. Panarella didn’t slow down—she went into overdrive to support survivors’ emerging needs.
For many survivors, recounting their story to a police investigator can bring up difficult memories and feelings. As a Senior Advocate, Ms. Panarella typically offers to meet survivors at precincts before they speak with an investigator. She explains the process to them and often sits with them during their interview. After the interview, Ms. Panarella helps them process their feelings. She also helps them navigate the criminal justice process, engage them in safety planning, refers them to counseling, helps them with practical resources like new locks for their home, and assists in applying for victim compensation.
During the COVID-19 crisis, social distancing protocols kept Ms. Panarella from sitting with survivors during interviews at precincts. But that didn’t stop her. She began to “accompany survivors” over the phone. She worked with a Brooklyn precinct to help manage the increased volume of domestic violence cases they were seeing. And she continued to follow up with the sexual assault clients she’d assisted before the pandemic, sometimes reaching out on a daily basis.
Ms. Panarella understood that the COVID-19 pandemic was contributing to stress and trauma, and she made sure her clients knew she was there for them.
“Jailene will always pick up the phone if someone calls her,” said Carmen Fleming, Senior Manager, Special Victims Division within CVAP. “She will do whatever is asked of her and whatever she can to help. She really, really believes in what she’s doing and really cares about the partnership with the police. She emanates so much passion for the job. That’s such a positive quality in this line of work.”
From Ms. Panarella:
“Growing up in New York City’s Public Housing, I have not only seen but have personally experienced many injustices throughout my life. My passion is to help people by listening to their stories, giving them options to find ways to support themselves, and voicing their concerns when they feel like their voices have been taken away, which is what continues to drive me to do this work.”
The Mayor’s Office of Community Mental Health program: Crime Victim Assistance Program
Before the Mayor’s Office of Community Mental Health, many crime victims navigated the complicated landscape of the criminal justice and social service systems alone. Just three precincts had one onsite victim advocate to serve victims of domestic violence. Now, victims of any kind of crime can be served by the Crime Victim Assistance Program, which operates in precincts and Housing Police Service Areas citywide and has served over 165,000 people since 2016. The program provides supportive counseling, connections to individual or group therapy, safety planning, assistance with victim compensation, and help navigating the legal and financial challenges that can emerge after a crime has occurred. During the COVID-19 pandemic, victim advocates provided remote support to people harmed by crime, violence or abuse. Learn more about the program and its impact here.
Stepping up for families in crisis
Catherine Maresco, Justine Stern-Beutler, Yolanda Rosado Ortiz, Julie Yates, Early Childhood Social Workers in the Bronx

Social workers are used to adapting to new circumstances – fast thinking and creative problem-solving are part of the job. But when the COVID-19 pandemic came to the Bronx, four Early Childhood Social Workers took adaptation to the next level.
Catherine Maresco, Justine Stern-Beutler, Yolanda Rosado Ortiz, and Julie Yates pride themselves in creating safe and nurturing classrooms for all kinds of young learners. They loved visiting classrooms, and offering support to teachers and students. But then the schools closed.
Almost overnight, children’s homes became the classrooms. On top of that, many of the families – and the staff – were in various forms of crisis, from sickness to parents losing their jobs.

Tragically, some families and school staff were mourning the loss of their loved ones.
Ms. Maresco, Ms. Stern-Beutler, Ms. Rosado Ortiz, and Ms. Yates adjusted to meet the profound need of the moment. They began sharing resources on self-care with parents and teachers. They set up regular online check-ins to make sure caregivers were also taking care of themselves. Where they could, they helped people in their community grieve, and helped children process their losses.
“Social workers work with children and families that may have had a loss, but not at this scale,” said Rudene Scipio, Mental Health and Wellness Administrator, Bronx. “These four have really stepped up to the plate.”
“Their dedication and commitment to the health and wellness of the Bronx community have shown that they are heroes,” continued Scipio. “And this remote work highlights it even more.”
From Ms. Maresco:
“Advocacy and support for one another, especially for those whose voices are often unheard, is most important to me. As an Early Childhood Social Worker, what keeps me motivated and inspired is the resilience of children and the strength of their families.”
From Ms. Stern-Beutler:
“I always focused on helping others by empowering them to bring about positive change in their lives. The successes that I have seen and my personal support systems – my family and my colleagues – give me the strength to continue to support others in need.”
From Ms. Rosado Ortiz:
“I strongly believe in the importance of addressing the social and emotional needs of children and families in our public-school system as part of my life-long commitment to work against the systemic cumulative economic, racial and social injustice in our marginalized communities of the Bronx, where I live.”
From Ms. Yates:
“I became interested in this work as a very young child due to my compassion, and intolerance of the suffering of marginalized and under-resourced people, and the continuous curiosity, and understanding of how to alleviate ills of society. I am relentlessly compelled after working in many areas of the developmental stages from early intervention to the elderly, as well as substance use; due to the pervasive injustice, and hypocrisy that continues racially, economically, educationally, and medically. In addition, I am compelled to work for positive change for: housing and food insecurity, care of the elderly, people with disabilities, the treatment of LGBTQ people; and the deliberate deletions, and inaccuracies (especially with the historical, and current education of our young learners) of the contributions that people of color have made, and continue to make to this country.”
The Mayor’s Office of Community Mental Health program: Social Emotional Learning
Social, emotional, and behavioral regulation skills are foundational for learning and well-being. Through a partnership between the Mayor’s Office of Community Mental Health and the Department of Education, Pre-K and 3-K programs across New York City provide social-emotional learning support to students, families, program leaders and teaching teams. Over 3,000 teachers and program staff participated in at least one professional learning session through this program since it launched in 2016. And, an additional 3,000 parents and caregivers have attended family workshops to learn social emotional development practices since 2016. Learn more about the program and its impact here.
Bringing support groups for teachers online
Barbara Biermann, an Early Childhood Social Worker in Manhattan
 In her role as an Early Childhood Social Worker for schools in Manhattan, Barbara Biermann has seen the value of nurturing the nurturers time and time again. That’s why, when schools closed to help stop the spread of the coronavirus pandemic, she knew immediately that it wasn’t just the students who needed support: the families and teachers who care for them needed help as well.
In her role as an Early Childhood Social Worker for schools in Manhattan, Barbara Biermann has seen the value of nurturing the nurturers time and time again. That’s why, when schools closed to help stop the spread of the coronavirus pandemic, she knew immediately that it wasn’t just the students who needed support: the families and teachers who care for them needed help as well.
Ms. Biermann began writing two newsletters—one for parents and another for teachers. She shared helpful tips on how to cope with new realities, including the switch to digital learning. In personalized emails chock full of resources, Barbara also normalized the stress and anxiety many teachers and parents were feeling.
It wasn’t the only time Barbara went above and beyond her usual responsibilities. In order to reach teachers in a variety of ways, Barbara created inter-school groups where teachers across multiple sites could connect and support one another. During the pandemic, Barbara convened these groups online so that teachers could continue to connect during the crisis.
“Barbara derives a lot of joy from helping people,” said Jodi Samson, Mental Health and Wellness Administrator, Manhattan. “She has a generosity of spirit and everyone who knows her feels enriched by having her in their community. When I told a teacher who knows Barbara that I nominated her as a hero, the teacher was so excited. It was obvious to her—who else would be nominated?”
From Ms. Biermann:
“As a social worker I am in a position to provide children, parents, and teachers a level of support they may otherwise be without.”
The Mayor’s Office of Community Mental Health program: Social Emotional Learning
Social, emotional, and behavioral regulation skills are foundational for learning and well-being. Through a partnership between the Mayor’s Office of Community Mental Health and the Department of Education, Pre-K and 3-K programs across New York City provide social-emotional learning support to students, families, program leaders and teaching teams. Over 3,000 teachers and program staff participated in at least one professional learning session through this program since it launched in 2016. And, an additional 3,000 parents and caregivers have attended family workshops to learn social emotional development practices since 2016. Learn more about the program and its impact here.